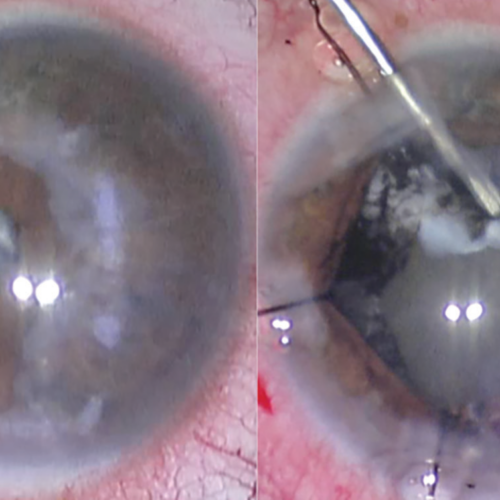
Having trouble seeing clearly after cataract surgery may be the result of a “secondary cataract.” Post-cataract surgery complications include posterior capsular opacification (PCO), sometimes called a secondary cataract or “after-cataract.” One of the most frequent after-effects of cataract surgery is posterior capsule opacification (PCO), the occurrence of which cannot be reliably predicted in individuals.
Capsular opacification often takes several years to develop; however, some patients may detect cloudiness weeks or months following cataract surgery. The good news is this may be easily remedied with a laser operation, allowing you to resume enjoying your normal level of vision.

If you’ve had cataract surgery and, weeks, months, or even years afterward, your vision has blurred or dimmed again, much like it did before, you may be wondering if your cataract grew back.
Cataract surgery involves the removal of the cloudy natural lens of the eye and its replacement with an artificial lens. Cataracts cannot develop on artificial lenses. What, then, maybe cause visual problems following cataract removal? While only an ophthalmologist can give you a definitive diagnosis, a secondary cataract may be to blame for your impaired vision after cataract surgery.
Explaining the term “secondary cataract.”
Some people may have temporary blurriness of vision after cataract surgery, despite the fact that cataracts cannot regrow. Thankfully, this is not another cataract and can be treated quickly and easily. Commonly called a “secondary cataract” or “after cataract,” the technical term for this condition is posterior capsular opacification (PCO).
To clarify, the term “secondary cataract,” understanding the eye’s structure is essential for answering this question.
The natural lens in your eye used to be encased in a little sac or membrane called the lens capsule, which kept it in place. Cataract surgery involves the removal of a significant portion of the capsule in front of the lens of the eye. The surgeon needs access to the hazy lens (caused by the cataract) in order to perform the necessary removal procedure. However, the portion of the membrane that covers the space behind the lens of the eye is left in place. After cataract removal, this area of the lens capsule can become foggy and may obscure vision in a few people. The cataract has not reappeared, despite what you may be feeling.
If you have a “secondary cataract,” what do you do?
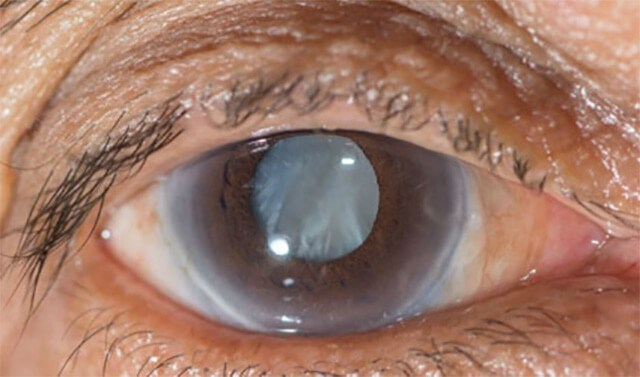
There have been reports of patients experiencing visual problems, including blurring or a general lack of brightness. Others claim to have trouble distinguishing colors, decreased near and distant vision, and are sensitive to light, especially at night. It is not another cataract, the phrase “secondary cataract” is only used to describe these experiences given that the symptoms are identical to those of cataracts. Such as:
- Perceived haziness or cloudiness in the eyes
- Vision impairment, especially at night, and trouble seeing in strong light conditions
- Seeing double images
The term “secondary cataract” sounds scary, but how exactly is it dealt with?
The cataract can be treated easily in cases of subsequent cataract formation. As an outpatient operation, YAG laser capsulotomy takes only a few minutes to complete and can result in nearly instantaneous improvement in vision. The technique causes no pain or discomfort because it does not involve an incision or contact with the eye.
The ophthalmologist performs a YAG laser capsulotomy to create a tiny incision in the back of the eye. With this slit, light may now enter the back of the eye without being dispersed or occluded, restoring clear vision.
Your vision may be slightly fuzzy following the treatment due to pupil dilation and broken-up capsule debris, but the effects are usually quick. It is common practice to schedule a follow-up consultation a week or two later to evaluate the eye’s pressure and your level of visual improvement.
Infections Caused by YAG Laser Capsulotomy
Patients seeking YAG laser capsulotomy to remove a secondary cataract should be aware of the risks associated with the surgery, as with any eye procedure. Increased optical pressure (IOP) inside the eyeball is the most typical cause. However, due to the rapid dissipation of laser energy from the eye, most patients with IOP recover to normal within 24 hours after the surgery. Postoperative IOP occurrences are particularly common in patients with glaucoma and other vision-threatening eye disorders; these patients will need closer monitoring. You can read about 10 Complications of Cataract Surgery and How to Cope with Them by visiting http://caiuk.org/10-complications-of-cataract-surgery-and-how-to-cope-with-them/
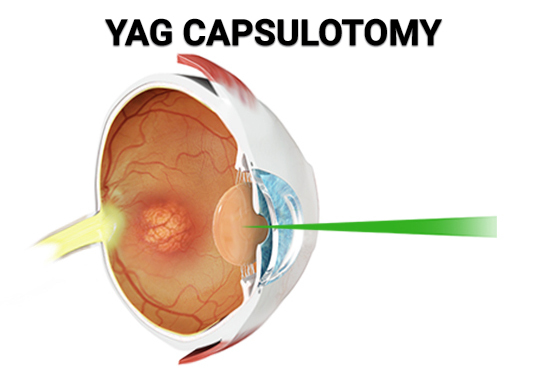
Although it is extremely unusual for patients to have any clinically significant eye pain or discomfort, anterior uveitis (inflammation inside the eye) is the second most common complication linked with YAG laser capsulotomy. Anti-inflammatory eye drops can be used to alleviate postoperative inflammation following a YAG capsulotomy, while most patients do not require therapy.
Retinal tears or detachments, which occur when the retina separates from the tissues that normally keep it attached, are a more dangerous but uncommon problem. Retinal detachment can also be brought on by trauma, severe diabetes, or retinal problems associated with aging. Contact an eye doctor immediately if you experience any of the following signs of retinal detachment:
Subtle particles that appear to hover in midair in the visual field might arise suddenly, and gradual peripheral vision loss can also occur. Light flashes in one or both eyes. Shadows that hang like curtains across the range of vision
An Alternative Method of Treating Posterior Capsular Opacification
To cure a secondary cataract, YAG capsulotomy is the only viable option. It’s possible that the capsule may continue to get thicker and more opaque over time, or that it will stay the same. Ultimately, the choice to have this operation is the same as the decision to undergo cataract surgery, in that it is dependent on factors like comparing the expense of the procedure against the benefit of clear vision. If you can get by without a YAG laser capsulotomy, then there’s no reason to have one done.
Is it possible to avoid secondary cataracts?
Secondary cataracts are more likely to develop in those who already have one of the following disorders. Those under the age of 40, those with diabetes, and those who suffer from uveitis (an infection of the central layer of the eye) or retinitis pigmentosa (a degeneration of the retina’s light-sensitive cells) are at greater risk. The use of steroids has also been related to “secondary cataracts.” Traumatic cataract sufferers may also be at a greater risk.
There is no way to prevent a “secondary cataract,” however advanced research in intraocular lens (IOL) design may lessen the likelihood of this complication. An example is a discovery that “square-edged” IOLs lessen the likelihood of getting a “secondary cataract,” yet they do not avoid it entirely. You can read more about secondary cataracts by clicking here.