Understanding LASIK Eye Surgery
LASIK (Laser-Assisted in Situ Keratomileusis) is a popular refractive eye surgery that corrects vision problems such as nearsightedness, farsightedness, and astigmatism. It aims to reduce a person’s dependency on glasses or contact lenses by reshaping the cornea.
Before diving into the key differences between bladeless LASIK and traditional LASIK, it’s important to grasp the basics of eye surgery LASIK as a whole.
The Basics of LASIK
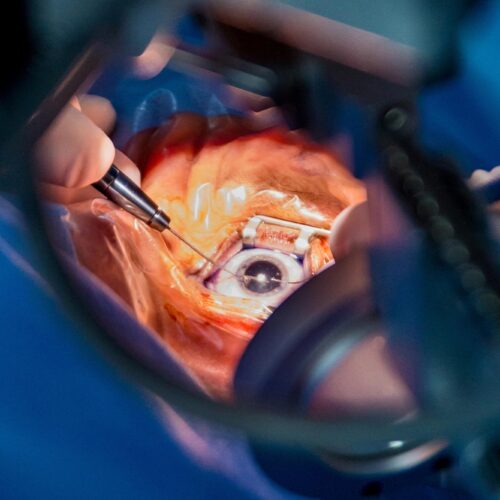
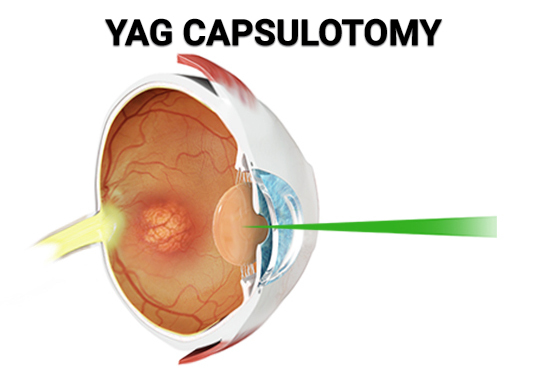
LASIK is a two-step procedure. First, a thin flap is created on the cornea using a microkeratome or a femtosecond laser. This flap is then lifted, exposing the underlying corneal tissue. In the second step, an excimer laser is used to reshape the cornea by removing a precise amount of tissue.
The reshaping of the cornea enables light to properly focus on the retina, resulting in clearer vision. It is a painless and quick procedure, usually lasting about 15 minutes per eye.
During the procedure, the patient’s eye is numbed with eye drops to ensure comfort. The surgeon then uses a specialized instrument to hold the eye open, preventing blinking and allowing for precise treatment. The laser is carefully calibrated to remove the correct amount of tissue, based on the patient’s unique prescription.
After the procedure, the corneal flap is repositioned, acting as a natural bandage. The eye typically starts healing immediately, with most patients experiencing improved vision within a few days.
The Evolution of LASIK Technology
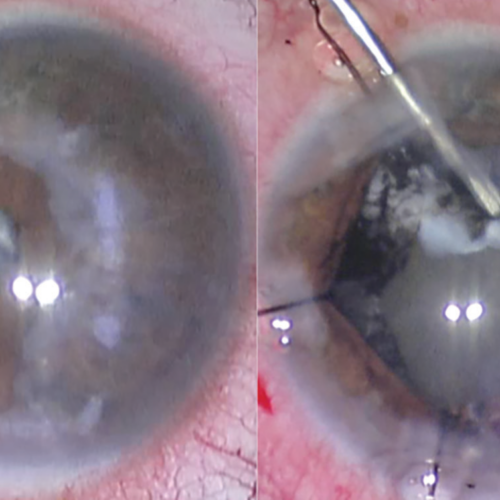
Over the years, LASIK technology has advanced significantly, leading to the development of bladeless LASIK. Traditional LASIK uses a mechanical microkeratome to create the corneal flap, whereas bladeless LASIK utilizes a femtosecond laser.
Femtosecond laser technology is known for its high precision and accuracy, providing surgeons with more control during the procedure. This technology has given rise to bladeless LASIK as an alternative to traditional LASIK.
In bladeless LASIK, the femtosecond laser creates the corneal flap with utmost precision, resulting in a more predictable and consistent outcome. This advanced technology has reduced the risk of complications and improved the overall safety of the procedure.
Furthermore, bladeless LASIK allows for customization based on each patient’s unique eye anatomy. The laser can be programmed to create a flap that best suits the individual’s corneal thickness and curvature, maximizing the effectiveness of the treatment.
Another advantage of bladeless LASIK is the reduced risk of flap-related complications. The femtosecond laser creates a flap with clean edges, minimizing the chances of irregularities or flap dislocations. This leads to faster healing and a smoother recovery process for the patient.
As technology continues to advance, LASIK surgery is becoming even more precise and tailored to individual needs. Surgeons are now able to perform wavefront-guided LASIK, which uses detailed measurements of the eye’s unique imperfections to guide the laser treatment. This further enhances the accuracy and quality of the vision correction.
In conclusion, LASIK surgery has come a long way since its inception. With the introduction of bladeless LASIK and other technological advancements, patients can now benefit from a safer, more precise, and customized procedure. LASIK continues to be a popular choice for those seeking freedom from glasses and contact lenses, providing them with clearer vision and an improved quality of life.
An In-depth Look at Traditional LASIK
Traditional LASIK is a widely practiced procedure that has been used for many years to correct vision. It involves the use of a handheld mechanical microkeratome, a cutting device with a small blade that moves back and forth, to create a corneal flap. This flap is then gently lifted to expose the corneal tissue for laser reshaping.
The use of a microkeratome blade in traditional LASIK has both benefits and risks. One of the main advantages is its relatively low cost compared to bladeless LASIK. This makes traditional LASIK a more accessible option for those who may not be able to afford the higher cost of bladeless LASIK.
Furthermore, traditional LASIK has a well-established track record, with many successful outcomes reported by patients. The procedure has been refined over the years, leading to improved techniques and better results.
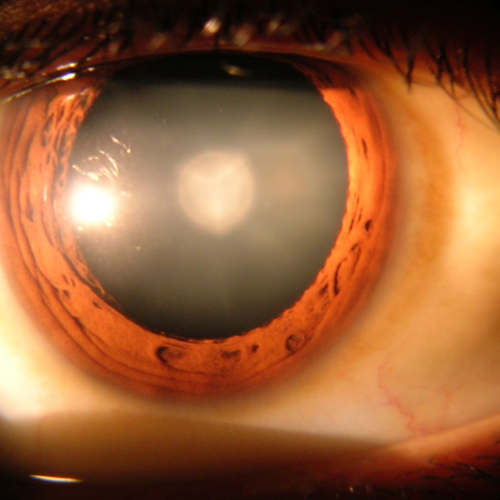
However, traditional LASIK does carry some risks. The use of a microkeratome blade introduces the possibility of flap-related complications. These complications can include partial flaps, buttonholes, and irregular flap surfaces. While these issues are rare, they may impact visual outcomes and require additional interventions.
Another factor to consider is the temporary discomfort and longer recovery times associated with traditional LASIK. The cutting action of the microkeratome can cause some discomfort during the procedure and may result in a slightly longer recovery period compared to bladeless LASIK.
It is important to note that the decision to undergo traditional LASIK should be made after a thorough consultation with an experienced eye surgeon. They will be able to assess your individual needs and determine whether traditional LASIK is the right option for you.
In conclusion, traditional LASIK is a well-established procedure that has been used for many years to correct vision. While it has its benefits, such as lower cost and a proven track record, it also carries some risks and may result in temporary discomfort and longer recovery times. It is essential to consult with a qualified eye surgeon to determine the most suitable treatment option for your specific needs. You can also read about Can You Get a Cataract After Cataract Surgery? by visiting https://caiuk.org/can-you-get-a-cataract-after-cataract-surgery/
Exploring Bladeless LASIK
The Procedure of Bladeless LASIK
Bladeless LASIK, also known as All-Laser LASIK or Femto LASIK, utilizes a femtosecond laser to create the corneal flap instead of a mechanical microkeratome. The laser precisely creates the flap with a high level of accuracy and customization.
The use of femtosecond laser technology eliminates the need for a blade, reducing the risk of flap-related complications. This makes bladeless LASIK an attractive option for those concerned about the potential risks associated with traditional LASIK.
Benefits and Risks of Bladeless LASIK
One of the major advantages of bladeless LASIK is its improved safety profile. The femtosecond laser allows for a more precise and predictable flap creation, reducing the risk of flap-related complications. It also offers a higher level of customization, allowing for individualized treatment plans.
Bladeless LASIK also tends to have a quicker recovery time compared to traditional LASIK. Patients often experience less discomfort and are able to return to their normal activities sooner.
However, it is important to note that bladeless LASIK may be costlier than traditional LASIK due to the use of advanced laser technology.
Comparing Bladeless and Traditional LASIK
When considering LASIK options, it’s important to factor in the cost. Traditional LASIK generally tends to be more affordable due to its longer history and wider availability. Bladeless LASIK may require a higher investment, but it offers the advantages of improved safety and precision.
Traditional LASIK has been around for several decades and has undergone extensive research and development. As a result, the procedure has become more streamlined and cost-effective over time. Many eye clinics and surgeons offer traditional LASIK as a standard option, making it more accessible to a larger number of patients.
On the other hand, bladeless LASIK is a newer technology that utilizes a laser to create the corneal flap instead of a microkeratome blade. This advanced technique offers increased safety and precision, as the laser can create a more precise and predictable corneal flap. However, the use of laser technology in bladeless LASIK can contribute to the higher cost of the procedure.
It is essential to consult with your eye doctor and consider your individual needs and financial situation when making a decision based on cost. Your doctor can provide you with a detailed breakdown of the costs associated with each procedure, including pre-operative evaluations, surgical fees, and post-operative care.
Recovery Time and Process
Recovery time can vary from patient to patient and depends on several factors, including the individual’s healing response and the complexity of their refractive error. However, in general, bladeless LASIK tends to have a slightly shorter recovery time compared to traditional LASIK.
After undergoing either traditional or bladeless LASIK, it is common to experience some discomfort and blurry vision for the first few days. However, most patients notice a significant improvement in their vision within the first week following the procedure.
Both procedures typically involve a post-operative care regimen that includes the use of medicated eye drops and regular follow-up visits with your eye doctor. These visits are crucial for monitoring your healing progress and ensuring that any potential complications are addressed promptly.
During the recovery period, it is important to avoid activities that may strain your eyes, such as reading for long periods or engaging in strenuous physical activities. Your doctor will provide you with specific instructions on how to care for your eyes during this time to promote optimal healing.
Long-term Results and Complications
When it comes to long-term results and complications, studies have shown comparable outcomes between bladeless and traditional LASIK. Both procedures have a high success rate in improving patients’ vision and reducing their reliance on glasses or contact lenses.
Many patients experience a significant improvement in their vision after LASIK, with the majority achieving 20/20 vision or better. However, it’s important to have realistic expectations and understand that individual results may vary.
It’s important to note that, as with any surgical procedure, there are potential risks and complications associated with both bladeless and traditional LASIK. These can include dry eyes, glare, halos, and under or overcorrection. However, the occurrence of complications is typically low and can be managed with proper post-operative care and follow-up visits.
Your eye doctor will thoroughly evaluate your eyes and discuss the potential risks and benefits of LASIK based on your specific circumstances. They will also provide you with detailed information on how to minimize the risk of complications and optimize your long-term results.
Making the Decision: Bladeless or Traditional LASIK
Factors to Consider
There are several factors to consider when deciding between bladeless and traditional LASIK.
First and foremost, it is essential to have a thorough consultation with your eye doctor. They will assess your specific eye condition, discuss your expectations, and recommend the most suitable option for you.
Cost, safety, customizability, recovery time, and personal preferences are among the other factors you may want to consider.
Consulting with Your Eye Doctor
Choosing the right LASIK procedure is a significant decision that should be made in consultation with your eye doctor. They are well-equipped to assess your individual needs and guide you through the decision-making process.
Be sure to ask any questions or address any concerns you may have during your consultation. Your eye doctor will provide you with the necessary information and support needed to make an informed choice.
In conclusion, both bladeless LASIK and traditional LASIK offer effective solutions for vision correction. The choice ultimately depends on your specific needs, preferences, and consultation with your eye doctor. With their guidance, you can choose the LASIK procedure that best suits your situation and take a step towards clearer vision.